There is one word that is used more in both describing and diagnosing back pain than any other word. This word is synonymous with back pain, however, it is used most of the time to describe a different problem than what the word actually defines. This has created many misunderstandings between patients and doctors and frequently confuses everyone when deciding how best to treat low back pain. This overused word needs to be properly defined if we are to move forward with proper diagnosing and treating of all low back conditions. What is the most overused word in back pain? It is the word sciatica.
Let’s define it!
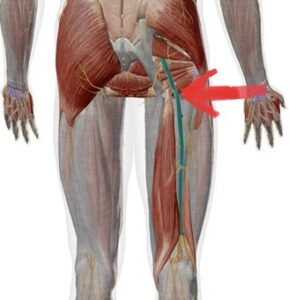
Sciatica by definition is nerve-like pain traveling down the back of one or both legs and into the toes. This pain pattern appears because the pain follows the sciatic nerve that travels down the back of the leg branching off into several smaller nerves below the knee. True sciatica follows the nerve route with pain radiating down past the knee frequently to the calf and toes.
 Nerve pain has an electric feel similar to when you hit your “funny bone” around your elbow. Many other conditions can cause sharp, shooting, dull, and achy pain to travel into the hip and down the leg but not past the knee. This pain pattern is not a sciatic nerve condition. More often these conditions involve the muscles of the hips, back, and around the knee. While these conditions are serious, they are not as clinically problematic as the true nerve pain that is related to sciatica.
Nerve pain has an electric feel similar to when you hit your “funny bone” around your elbow. Many other conditions can cause sharp, shooting, dull, and achy pain to travel into the hip and down the leg but not past the knee. This pain pattern is not a sciatic nerve condition. More often these conditions involve the muscles of the hips, back, and around the knee. While these conditions are serious, they are not as clinically problematic as the true nerve pain that is related to sciatica.
Where is it?: Let’s take a closer look at specifics of true sciatica. Do you know where the sciatic nerve runs? The sciatic nerve starts in the low back in the spinal cord from levels L4-S3 and runs down the gluteal region near the piriformis (possibly through or splitting it) down the back of the leg. True sciatica is when that nerve gets entrapped (smashed) by any of these muscles or the intervertebral discs. Each of these entrapments will cause nerve pain in different places in/on your lower leg. True sciatica will cause pain on the outside of the calf and back of the leg (not hamstring) along with the top, bottom, and outside of the foot.
Sciatic Symptoms:
- Pain that is sharp, electric shock-like, numb, or deep and achy
- Pain that is mostly constant
- Pain that is along the distribution of the nerve (in the back, buttock, and leg)
- Pain that is almost always only down 1 leg, not both
- Pain that goes past the knee
- Walking difficulties
- Decreased power in the leg
- Decreased reflexes
Many people will have pain on the side of the thigh, back of the hamstrings, and possibly down into the leg and foot. These symptoms are more related to radiculopathy, which is when a spinal nerve gets entrapped/injured in your low back most often by the intervertebral discs. These specific areas of pain often help lead us to our diagnosis and can cause us to alter our treatment and rehab recommendations.
Why:
“I don’t know what I did, it just started shooting down my leg,” or “I just was trying to tie my shoe and it started,” are common phrases when people describe how their pain started. In fact, most people with sciatica can not pinpoint one specific event that led to their pain. This is due to the fact that most sciatic cases are due to repetitive motions and forward bending behaviors. These behaviors create a disc bulge in the lower lumbar spine, causing the muscles in the hips to tighten around the sciatic nerve, or a combination of both to cause the sciatica over a lengthy period of time.
Very few low back cases begin with trauma; most cases are created by similar frequent activities. That is why I prefer to see back pain as more of a behavioral problem than a structural problem. As mentioned above, sciatica will only cause pain in the leg. Other causes of low back pain could be lumbar spine facet joints, muscle strains, or sprained SI joints. Likewise, these causes of back pain are frequently created by repetitive motions and behaviors. Sitting, bending, over stretching, over training, bad sleeping positions, and driving are a few of the more common behaviors that lead to sciatica and other low back conditions. In the rare and emergency case, DVT (deep vein thrombosis) typically causes calf pain and swelling. This is an emergency case that should not be ignored. As always, if you think what you are experiencing is a true emergency, call or go to the emergency department.
Other considerations: There are many concerns about properly diagnosing back conditions with x-ray and other imaging studies. First, you can not see sciatica on an x-ray. Muscles, discs, or ligaments do not appear on an x-ray. The only thing that can be visually seen on an x-ray is bone and spaces between bones.
 Second, research shows that many people with no low back pain will have disc bulges or protrusions seen on an MRI. Also, most MRI’s are taken laying down, which takes some of the pressure off the disc. This means that a sciatica causing disc bulge could possibly not show up on an MRI. That is why it is extremely important to have a knowledgeable physician do a thorough hands-on functional evaluation in the office and not exclusively depend on imaging. Imaging is a great tool, when used in the correct context, but it is not always necessary. Often orthopedic and neurological tests combined with functional movement screens that we perform in our office tells us what we need and how we need to treat the patient. However, if imaging (x-ray, MRI, etc) is needed, we are able to order them.
Second, research shows that many people with no low back pain will have disc bulges or protrusions seen on an MRI. Also, most MRI’s are taken laying down, which takes some of the pressure off the disc. This means that a sciatica causing disc bulge could possibly not show up on an MRI. That is why it is extremely important to have a knowledgeable physician do a thorough hands-on functional evaluation in the office and not exclusively depend on imaging. Imaging is a great tool, when used in the correct context, but it is not always necessary. Often orthopedic and neurological tests combined with functional movement screens that we perform in our office tells us what we need and how we need to treat the patient. However, if imaging (x-ray, MRI, etc) is needed, we are able to order them.
It is often said that “If you want a reason to operate on something, do an MRI]” MRI’s are the gold standard of imaging, but an MRI is only as good as the history and exam findings. Both MRI and exam findings must point to a similar diagnosis.
How can we help:

 Sciatica can come from a variety of sources, and it is important to try and determine the most likely source. This is because, depending on the source, the management can be completely opposite. For example, if you have sciatica due to a disc herniation pressing on the L5 nerve root, then you will likely prefer extension-type exercises.
Sciatica can come from a variety of sources, and it is important to try and determine the most likely source. This is because, depending on the source, the management can be completely opposite. For example, if you have sciatica due to a disc herniation pressing on the L5 nerve root, then you will likely prefer extension-type exercises.
However, if you have sciatica from spinal stenosis, then you will likely prefer flexion-type exercises. Additionally, if you do the opposite exercises than what would be most preferable, you may actually make yourself worse!
If you think you may have sciatica, one exercise you can do to try and improve how well your nerve is moving is called a sciatic nerve floss.
Here’s a good Sciatic Nerve Floss Video:
Remember to look up as you bend your foot, and look down as you straighten your foot. Timing is important, and doing it opposite (i.e. bending foot up while looking down), can make you more irritable. You should only complete this exercise if it feels relieving or if it feels like a “nothing” feeling. If it hurts, stop, and ask us for assistance.
At our office we see all of the symptoms listed above on a daily basis. We often look at the body in a different way than other providers. Our goal is to not only reduce your pain but figure out what the problem is and teach you ways to help yourself now and in the future. The techniques and rehabilitation we use in our office focuses on the long term goal which is to help lessen the chance of the injury coming back. Our tests done in the office lead us to how we are going to treat the patient and how we can help them.
We use a variety of adjusting techniques, soft tissue therapy, acupuncture, and therapeutic rehabilitation. Often our patients go home with a simple, yet specific exercise/movement to be able to improve at home. We provide hands-on care that assesses your biomechanics, minimizes risk of injury, and exceeds your healthcare goals. We strive to educate our patients so that they understand what is going on and how they can help themselves feel better. Our goal is to see each patient become healthier than they have ever been.







